Creating time
for better care
AI-powered medical
intelligence for
Trusted by 1000+ healthcare units






Less admin & better use of resources
Faster response
More satisfied staff and patients
Klinik.ai is powered by our CE-marked medical engine. It is a medically supervised patient access & triage software that recognizes thousands of symptoms and conditions. It indicates the urgency level of patients’ symptoms and provides pre-diagnoses for healthcare professionals.
Offered as an embedded solution for our partners’ digital systems, Klinik.AI seamlessly integrates medical intelligence into existing platforms and workflows — reducing admin, optimizing resources, and enabling faster, better patient care.
The medical engine has been in use since 2015 in multiple countries and has proven to be safe and accurate
>1000
0–120yrs
> 10 years
Over 22 million
> 5,000
> 1000
Klinik.AI has a proven track record as an embedded solution for a wide range of partner companies.
Bringing Value to Partners
We bring value to our partners through a deep understanding of patient flows, helping improve and automate professional workflows. By elevating user experience while ensuring medical accuracy and patient safety, we lead with strong insights derived from unique, medically rich data.
Supporting Our Partners
We support our partners by designing joint propositions and solutions tailored for end customers, ensuring seamless integration of solutions, and providing professional onboarding and ongoing support. At the same time, we focus on developing partnerships with a futureproof AI product pipeline.
Our Way of Operating
Our way of operating is centered on creating joint value propositions for both current and new customers. We embed AI components into partner solutions, strengthen competitive edge and market leadership, and open opportunities to create new revenue streams.

Klinik AI is a partner-focused healthtech company delivering AI-powered solutions that can automate the initial stages of any patient care journey.
We enable our partners to provide greater value to healthcare providers by improving access, efficiency, and clinical outcomes—creating time for better care.
01
Our Vision
02
Our Mission
03
Our Legacy
Klinik AI is a proven solution with vast experience and usage across multiple markets.
Roxbourne Medical Centre
Roxbourne Medical Centre
News
The 4-Week Pivot: How to Launch Clinical Triage Without Rewriting Your Codebase
You want triage in your product, but you don’t want to blow up your roadmap to get it. That tension sits at the heart of almost every health tech strategy conversation today, especially if you sell into larger provider networks or global health systems.
This is where the 4-week pivot matters: you launch clinical triage as embedded infrastructure, not as another fragile feature welded into your codebase. You keep your architecture, roadmap, and velocity. You add a clinically proven, CE-marked engine that your customers treat as part of your platform.
Your primary keyword here is simple: clinical triage.
Supporting keywords:
- embedded triage
- supplier-first model
- iframe integration
- CE-marked engine
You are not buying a widget. You are shifting where clinical logic lives in your stack.
The speed problem you feel every quarter
Every roadmap session starts to sound the same.
- Sales wants a triage story to stop losing deals to competitors that “go deeper into workflow”.
- Customers want richer clinical capability, not another booking form.
- Procurement wants evidence, CE marking, and governance artefacts.
- Engineering wants a stable scope that doesn’t drag them into medical risk.
And you sit in the middle, watching the same pattern repeat:
- A key account asks for triage or “more intelligent” intake.
- Product sketches options but sees nine to twelve months of build, validate, and certify.
- Compliance explains what clinical safety actually involves.
- Everything slows down. The feature gets re-scoped, pushed, then quietly dropped.
By the time you revisit triage, your competitors have changed the reference point in the buyer’s head. You still have a nice UX; they have a workflow story.
The problem is not a lack of ambition. It is the assumption that adding clinical triage must mean:
- new data models
- new logic layers
- new risk assessments
- a fresh CE-marking or equivalent safety process
Under traditional build logic, that assumption is rational. When you compile clinical reasoning into your codebase, every change becomes a regulated event. Release cadence bends around safety, not speed.
But your product does not need to own medical reasoning. It only needs to host it.
The quiet assumption that keeps you stuck
Most teams inherit the same unspoken rule:
“Clinical workflows belong inside the product.”
That rule made sense when the only way to add triage was to build your own engine or bolt on a separate app. Both paths came with cost:
- Build: You take on medical logic, governance, and regulatory duty of care.
- Bolt-on app: You fragment the workflow and force users into yet another system.
Both options slow you down and introduce friction. So triage stays on the “later” list, and sales keep explaining “we don’t do that yet.”
But the rule is wrong. Clinical workflows do not have to live inside your codebase. They need to live close enough to feel native, and far enough away to keep risk and complexity out of your stack.
That is where embedded infrastructure shifts the game.
What “embedded infrastructure” actually means
Embedded infrastructure treats clinical triage as an external, white-label engine you plug into your product rather than something you own and maintain line by line.
The pattern looks like this:
- Your database remains unchanged.
- Your backend stays intact.
- Your UI hosts an embedded, configured triage interface via an iframe.
- Your users move through your brand, your navigation, your flows.
On paper, this sounds simple. In practice, it solves three hard problems at once.
- Risk isolation
The clinical engine runs in a CE-marked environment, governed and updated by a medically-led team. Your codebase does not become a medical device. Your release process stays aligned to software, not safety-critical tooling. - Compliance containment
Clinical evidence, validation, and audit trails live with the engine provider. You inherit them as documentation and assurance, not as work you have to redo from scratch. - Workflow ownership
You still design the journey. You decide where triage appears, how outputs route into scheduling, messaging, or case management, and how your analytics interpret those outputs.
Technically, this is old-school web tech: iframes. Strategically, it is a modern supplier-first play.
Iframe deployment looks unfashionable if you assume it is only for static content. In healthcare, it delivers isolation where you need it most:
- Regulatory updates happen in the engine, not your app.
- Clinical content changes do not trigger your release cycle.
- You skip the “re-open ISO, re-open safety case” every time guidance changes.
You own the experience. You outsource the liability-laden logic.
Why embedded triage unlocks speed
When triage logic lives outside your product, your team gets to be a product team again.
You focus on:
- Experience design.
- Feature sequencing.
- Commercial differentiation.
- Onboarding, adoption, and outcomes.
Meanwhile:
- Clinical governance sits with a team whose full-time job is to maintain and extend a CE-marked engine.
- Compliance teams review supplier documentation and risk-sharing arrangements instead of authoring everything from scratch.
- Regulatory updates in the engine land as configuration changes to you, not rebuilds.
The effect is simple: you stop trading velocity for safety.
And because the engine is already in production elsewhere, you do not prove from zero. Klinik AI, for example, has been in clinical use for over 10 years, across more than 22 million patient cases and 5,000 professionals in over 1,000 units. That history becomes part of your story.
Dr Rony Lindell, Medical Director at Klinik and practising GP, frames the opportunity clearly:
“AI has the potential to introduce critical efficiencies, save on clinical time, and support clinical decision making but only if clinicians understand what’s possible, and what’s needed, both from the technical and human sides, to integrate AI into existing workflows and systems.”
You are not just embedding code. You are embedding the lived experience of a clinical system that has already been battle-tested.
The 4-week pivot: what actually happens
You want to know the actual clock time. Not “in principle”. Not “assuming no blockers”.
The 4-week pivot is designed around what you control, not what you hope for.
Week 1 – Technical alignment
You bring your engineering and product teams together with the engine provider.
The work here is concrete:
- Identify the surfaces where triage will live in your product.
- Decide iframe placement, sizing, and responsive behaviour.
- Confirm authentication patterns: JWT, SSO, session management.
- Agree data handover points for triage outputs, such as urgency, suggested diagnosis group, and routing recommendations.
- Lock down styling: typography, colours, spacing, and tone so the experience feels native.
You do not redesign your architecture or overhaul your schema. You map existing objects patients, tickets, encounters to the triage output fields you want to consume.
At this point, your engineers see something vital: the blast radius is small.
Week 2 – Embed and configure
This is where the engine appears inside your product for the first time.
The core steps:
- Add the iframe component into your front-end.
- Wire authentication to pass only the minimum necessary context.
- Configure clinical flows relevant to your buyers: primary care, MSK, mental health, or multi-specialty, depending on scope.
- Apply your brand theme and language to labels, instructions, and transitions.
The medical reasoning is already built. Klinik’s engine, for instance, recognises over 1,000 diagnoses and symptoms with age coverage from 0 to 120 years, including paediatrics, dental, and obstetrics. You are selecting and shaping, not authoring clinical content.
By the end of week 2, internal users can run through end-to-end journeys in a staging environment and see live outputs.
Week 3 – Connect workflows
Now you make triage matter operationally.
You decide how outputs feed your existing features:
- Urgency maps to queue priority, SLAs, or appointment templates.
- Proposed diagnosis clusters drive routing to GP, nurse, pharmacist, physiotherapist, or digital follow-up.
- Red-flag indicators trigger safety escalations or alerts.
- Structured clinical history populates your consultation view so clinicians see a clear picture before contact.
You also connect triage data to your reporting or analytics modules:
- Demand by condition group.
- Urgency mix over time.
- Resource load by clinician type.
- Channel distribution: web, phone-assisted, or walk-in captured as equivalent.
This turns triage from a “feature in the corner” into the engine of your product’s value story: demand management, resource optimisation, and equity.
Week 4 – Launch readiness
The final week is less about code and more about confidence.
You work across:
- Compliance: map your risk register to the supplier’s safety case, CE mark documentation, and incident management process.
- Information governance: clarify data flows, hosting, and role boundaries for DPIA or equivalent responses.
- Sales enablement: craft narratives, demo flows, and objection handling for “Is this safe?”, “How is it regulated?”, and “How does it treat vulnerable patients?”.
- Customer success: build onboarding playbooks and adoption dashboards that point to early wins.
Because the underlying engine is already certified and used at scale, you show buyers real impact data instead of hypothetical benefits.
Priory Medical Group, for example, used Klinik to see 8,000 more patients over a period, increasing throughput from 35,000 to 43,000 with the same staffing level. They cut routine wait times from four weeks to around 5–6 working days and dropped Did Not Attend rates from 5% to 1%.
Their managing partner, Martin Eades, puts it plainly:
“We are seeing 8000 more patients … with the same level of resources thanks to Klinik. Waiting times for routine receptions fell from 4 weeks to 5–6 working days and DNAs from 5 to 1.”
You take that story into your sales deck on day one.
Four weeks. No rebuild. No new medical device status for your codebase. No lost momentum.
How embedded triage flips compliance from blocker to asset
Most health tech launches stall on compliance, not code.
The classic pattern:
- You design an elegant intake or triage flow.
- You prototype quickly in your existing stack.
- Then you hit CE marking, or equivalent local safety standards.
- Timelines stretch. Risk registers grow. Everyone gets nervous.
Embedded infrastructure changes who does the heavy lifting.
With a pre-certified engine:
- Clinical risk is managed within a framework that already satisfies regulatory expectations.
- Safety evidence, validation reports, and ongoing surveillance are maintained by the engine provider.
- You inherit those artefacts via contracts, documentation, and governance packs rather than recreating them.
For buyers, this matters more than architecture diagrams. They ask three questions:
- Is it safe?
- Is it proven?
- Who is on the hook when something goes wrong?
A supplier-first engine like Klinik answers with:
- A CE-marked medical device, in operation for over a decade, across millions of cases.
- Clear lines of responsibility between medical governance and product ownership.
- A safety story that fits procurement templates and clinical risk committees.
Compliance stops being the reason you delay triage. It becomes the reason buyers trust your triage story.
Revenue follows capability, not slides
You feel the revenue drag when triage is absent.
- Enterprise deals stall at the same stage with the same question: “How do you handle urgency and demand?”
- RFPs mark you down on clinical capability and equity of access.
- Sales calls end with “We like you, but we need more workflow depth.”
Once triage becomes part of your live product, three things happen:
- Sales stop apologising
Your team no longer promises “phase two” builds they know will not land this quarter. They show working workflows, live routing, and real data. - Enterprise deals speed up
Health system buyers want systems that manage patient flow, not just appointments. When you demonstrate intake, prioritisation, and smart routing, you answer the brief out of the gate. - Custom builds decrease
Instead of bespoke “can you build us X?” requests, you steer buyers into standardised, configurable triage patterns that already meet safety expectations.
The result is direct: higher contract values, shorter sales cycles, and fewer distractions for your engineering team.
What buyers actually care about in triage
Buyers rarely want to read the algorithm spec. They care about outcomes, governance, and fairness.
The core questions you need to answer:
- Does it work in real clinics, at scale?
- Does it treat vulnerable and digitally excluded patients fairly?
- Does it integrate with existing workflows and systems?
- Does it help them survive demand, not just tidy it?
An embedded engine like Klinik gives you concrete answers:
- Over 22 million patient cases triaged, with structured symptom capture, urgency decisions, and differential diagnoses.
- Channel-neutral data capture so the same structured assessment applies whether the patient uses a web form, calls via an assisted telephone module, or walks in.
- Routing logic that directs cases to the most appropriate professional, rather than defaulting everything to a GP.
- Network-ready hub models for multi-site providers where demand can be balanced across practices.
You show, not just tell. In a demo, you run a live journey, then flip to a demand dashboard that shows how that single request enters a larger demand picture.
Equity and access as built-in behaviour, not a slide
Modern health system tenders weigh equity heavily.
You are expected to show that your product:
- Does not favour digital-first patients over those who use the phone or walk in.
- Does not reward those who log on at 8:00 sharp over those who struggle to access services.
- Does not lock out older adults or non-native speakers.
Generic “digital front doors” often fail here. They widen gaps.
They:
- Increase complexity for staff.
- Confuse patients.
- Create hidden triage nodes where admin teams make clinical decisions without proper support.
Klinik’s engine tackles this structurally:
- Clinical necessity, not arrival time
Urgency is based on medical need, not who clicked first. - Channel neutrality
Whether a patient is 20 and using an app, or 90 and on the phone, the system captures the same structured clinical information and runs it through the same engine. - Standardised assessment
Every patient is assessed using the same clinical framework, reducing variation and bias introduced by ad-hoc questioning.
When you embed this, you are not just adding a feature. You are embedding a defensible equity story into your product. And when bid teams ask you to prove it, you show the logic, not just the language.
Scaling across networks without rewriting anything
If you sell into multi-site providers, networks, or integrated care systems, you know the pain: what works in one practice breaks across ten.
The reasons:
- Each site has its own triage culture and process.
- Data lives in silos.
- Demand and capacity are invisible at network level.
A hub-ready triage engine changes that.
Klinik’s hub model uses embedded triage to create:
- Centralised triage
A single digital hub where a shared team manages enquiries for the entire network. - Network-level load balancing
If one practice is overloaded and another has capacity, cases can be routed across sites, not just within one clinic. - Standardised pathways
Patients get comparable clinical assessments regardless of their registered surgery. - Strategic visibility
Dashboards show real-time demand and capacity across the network, supporting staffing and planning decisions.
You embed the same engine once, then configure it for networks rather than re-building logic in each customer’s environment.
This is where your product shifts from “app” to “infrastructure” in the buyer’s mind.
Your roadmap, still yours
A legitimate fear: if you bring in an external engine, do you lose control?
You keep control where it matters:
- You decide when and where triage is surfaced.
- You define which outputs your system uses and which it ignores.
- You design the flow from symptom entry through to booking, messaging, or remote care.
The clinical engine sits behind a contract and an iframe. Your product strategy stays in-house.
That balance externalised risk, internalised control—is the core of the supplier-first model.
One pattern, many suppliers
The story repeats across digital front doors, telehealth platforms, patient portals, EPR vendors, and specialist tools.
A typical example:
- A digital front door supplier is losing deals because it lacks robust triage.
- Internal estimate: nine months to build a safe engine, plus unknown time for CE marking and governance.
- Instead, they embed a CE-marked engine via iframe.
- In four weeks, they ship clinical intake, urgency detection, and routing tightly integrated into their UI.
Their sales team re-opens stalled opportunities with working triage in the demo environment. Their product team goes back to building differentiated value on top of that infrastructure.
Internally, the conversation shifts from “Should we build triage?” to “Where else does this data let us lead?”
How Klinik AI positions you as infrastructure, not a feature
Klinik AI does not compete with you for provider relationships. It is built as supplier-first revenue infrastructure.
That matters for three reasons:
- No channel conflict
Klinik does not go direct to practices in a way that undercuts your sales. Its commercial model is built around empowering suppliers, not bypassing them. - White-label by design
The iframe integration is fully white-labelled. Patients see your brand, not a third-party logo carousel. - Supplier economics
The value proposition is tuned to your metrics: faster time-to-revenue, increased ACV, and reduced risk.
If you want to dig into the strategic framing or explore more build-vs-buy angles, three useful internal perspectives from the same content set are:
- Hidden compliance tax of building your own triage engine.
- Why your enterprise deals are stalling it’s not your UI, it’s your workflow.
- The end of the monolith and the rise of modular health tech.
Taken together, they reinforce the same point: own the experience, embed the clinical infrastructure.
Practical next steps if you are serious about a 4-week pivot
If you want clinical triage in production this quarter, treat it like any other focused initiative.
- Decide the minimum viable triage scope
- Channels: web only, or web plus phone-assisted input.
- Clinical domains: start with general primary care, or include specific modules like MSK.
- Outputs you will actually use: urgency, routing, structured history.
- Run a technical spike with your engineering team
- Validate iframe constraints in your front-end stack.
- Map authentication and authorisation boundaries.
- Identify how triage outcomes map into your data structures.
- Engage your governance lead early
- Share CE-mark documentation, safety cases, and DPIA-related material.
- Clarify how incident reporting and clinical oversight work.
- Position this as risk reduction, not risk introduction.
- Arm your sales and CS teams
- Build a simple narrative: “We manage demand, not just appointments.”
- Use real-world Klinik data like the Priory Medical Group outcomes to signal what’s possible.
- Create one high-impact demo flow from symptom entry to clinical routing.
- Plan your first lighthouse customer
- Choose a site or buyer with clear pain and leadership buy-in.
- Define what success looks like in 90 days: wait times, throughput, or staff workload.
- Commit to sharing outcomes as part of your market story.
You are not betting the company. You are running a controlled, high-leverage experiment with a proven engine.
Frequently asked questions
1. How safe is an embedded triage engine compared to building our own?
A mature engine like Klinik is CE-marked, medically supervised, and has triaged over 22 million cases across more than 1,000 units, with continuous monitoring and governance. An internal build would need to replicate that level of validation and oversight from a standing start.
2. How does iframe integration work with security and IG requirements?
Iframe-based deployment keeps the clinical engine in a controlled environment while your product passes only necessary context and receives structured outputs. With clear DPIA documentation, data processing agreements, and technical controls, this aligns with health system security expectations.
3. Will clinicians trust AI-driven triage?
Clinicians build trust when they see consistent, accurate outputs and clear safety boundaries. Klinik combines structured AI interviews, transparent urgency decisions, and negative symptom screening to give triage teams a clear clinical picture before contact, which reduces scepticism.
4. How does embedded triage support digital equity?
Klinik captures identical clinical information across online, telephone-assisted, and walk-in channels, then applies the same engine to every case. That channel neutrality ensures access is based on medical necessity rather than time of contact or digital literacy.
5. Can this model scale across multi-site providers or networks?
Yes. Klinik’s hub model enables centralised triage, load balancing across practices, and unified demand and capacity dashboards at network level. You re-use the same engine while configuring workflows per site or network, without rewriting your codebase.
6. What measurable impact should we expect our customers to see?
Real-world examples show significant capacity and access gains: Priory Medical Group handled 8,000 more patients with the same resources, cut routine wait times from four weeks to 5–6 working days, and reduced DNA rates from 5% to 1%. Your exact numbers depend on baseline demand and how you route outputs into your workflows.
Why the build vs buy decision is harder in healthcare AI
In most SaaS categories, building a feature in house is a straightforward trade‑off between time, cost, and flexibility. In healthcare AI, especially triage, the trade‑off adds three extra dimensions:
- Clinical safety and liability
- Regulatory exposure
- Long‑term maintenance and governance
You are not just deciding whether you can build the logic. You are deciding whether you want to live with:
- How that logic behaves in edge cases.
- How clinicians around the world use it under pressure.
- How regulators in different jurisdictions interpret it over time.
This is why many organisations report that the barriers to AI adoption are not purely technical but include regulatory uncertainty and concerns about the maturity and risk of AI tools.
What you are really building when you build triage
You might think you are building a symptom checker. In practice, you are building:
- A clinical decision support system that can fall under medical device rules.
- A global clinical knowledge base that must stay up to date.
- A risk classification engine that handles varied populations and comorbidities.
- A continuous validation pipeline to prove safety in real‑world use.
- A governance and audit function to satisfy hospital, insurer, and regulator questions.
Different regions name the rules differently – for example, FDA guidance for clinical decision support, EU MDR, or national digital health regulations – but the direction of travel is the same: more scrutiny on software that guides clinical decisions. That scrutiny does not disappear just because your team calls it “a feature”.
The global compliance tax nobody scopes
The compliance tax is not a one‑off project. It is an ongoing operating cost that grows with your footprint.
When you build triage in house, you commit to:
- Clinical validation
Showing that your logic behaves safely across age ranges, conditions, and care settings, and updating that evidence as you expand into new markets. - Safety documentation
Producing artefacts that can stand up in front of hospital risk committees, quality teams, and, where applicable, regulators. - Post‑deployment surveillance
Monitoring outcomes, investigating incidents, and demonstrating how you improve the system over time. - Change management
Accepting that every “small tweak” to logic affects a regulated risk surface and may require review, regression testing, and new documentation.
Global expansion multiplies this tax.
What passed a procurement review in one country may raise new questions in another. Two regulators can classify similar software at different risk levels, with different expectations, for the same functionality.
Internal teams consistently underestimate this. Surveys of healthcare organisations highlight regulatory uncertainty, lack of clear governance, and concerns about immature tools as top barriers to AI adoption. Those same issues become your problems the moment you own the triage engine.
Why engineering velocity collapses as you scale
The first version of an internal triage engine usually ships fast:
- Hard‑coded rules.
- Simple branching.
- Manual testing.
Then real requests arrive:
- Cover more age ranges and vulnerable groups.
- Support additional specialties or care settings.
- Adapt flows to fit different provider workflows and cultures.
- Address feedback from clinical champions in each new deployment.
Each change introduces new interactions in your logic and new risk paths to consider. Over time:
- Release cycles slow down because each change requires deeper testing.
- A small group of engineers and clinicians get pulled into constant triage maintenance.
- Roadmaps shift from strategic features to reactive fixes and compliance work.
What started as “two engineers for a quarter” becomes a permanent team whose main job is keeping the triage engine safe, documented, and just good enough to avoid blockers in deals.
The opportunity cost for global health tech teams
The real cost of building triage is not just regulatory work. It is what your team stops doing.
Your competitive edge in global healthcare markets tends to live in:
- How well you integrate into local workflows and systems.
- How you support different care models across countries.
- How you handle multi‑site, multi‑region deployment and analytics.
- How strong your commercial model and distribution are.
Customers rarely choose a platform because its homegrown symptom tree is slightly different. They choose it because:
- It reduces admin and improves capacity.
- It fits how their teams work.
- It meets their risk and compliance expectations without endless negotiation.
Every sprint spent rewriting triage logic for a new country is a sprint not invested in better integrations, better data, or stronger partnerships.
Why triage is infrastructure, not your differentiator
In global healthcare, triage behaves like infrastructure:
- It must be safe.
- It must be consistent.
- It must be predictable and explainable.
That is why more providers and payers expect triage and clinical decision support to meet medical device‑level standards, even where the exact regulatory status varies.
Your defensible IP is far more likely to be:
- The way you orchestrate workflows around triage outputs.
- How you align with each market’s operational reality.
- How you surface insights about demand and capacity to leaders.
- How easy you make it for clinicians to trust and use your product day to day.
Triage itself is a critical building block, but in a global strategy it behaves more like cloud infrastructure or payments than like your core UX.
The real risk when triage goes wrong
When triage fails, the consequences are serious everywhere:
- Patients may be under‑triaged or over‑triaged.
- Clinicians may lose trust in both the tool and your brand.
- Providers may face investigations, and you may be pulled into them.
- Regulators and payers may raise questions that affect future deals.
Studies of AI triage and risk prediction tools in emergency and referral settings highlight the ethical and practical challenges around over‑triage, under‑triage, false positives, and automation bias. These are not abstract issues; they influence how decision makers treat any new AI‑driven triage solution.
Even in jurisdictions where certain decision support software is not tightly regulated, commentary stresses that developers still need robust validation and transparency because oversight frameworks are evolving.s
If you own the triage engine, you own that risk narrative in every market you enter.
Build vs buy: how the comparison changes globally
The naïve calculation:
- Build: engineering cost for a few months.
- Buy: recurring licence plus integration.
The more accurate global calculation:
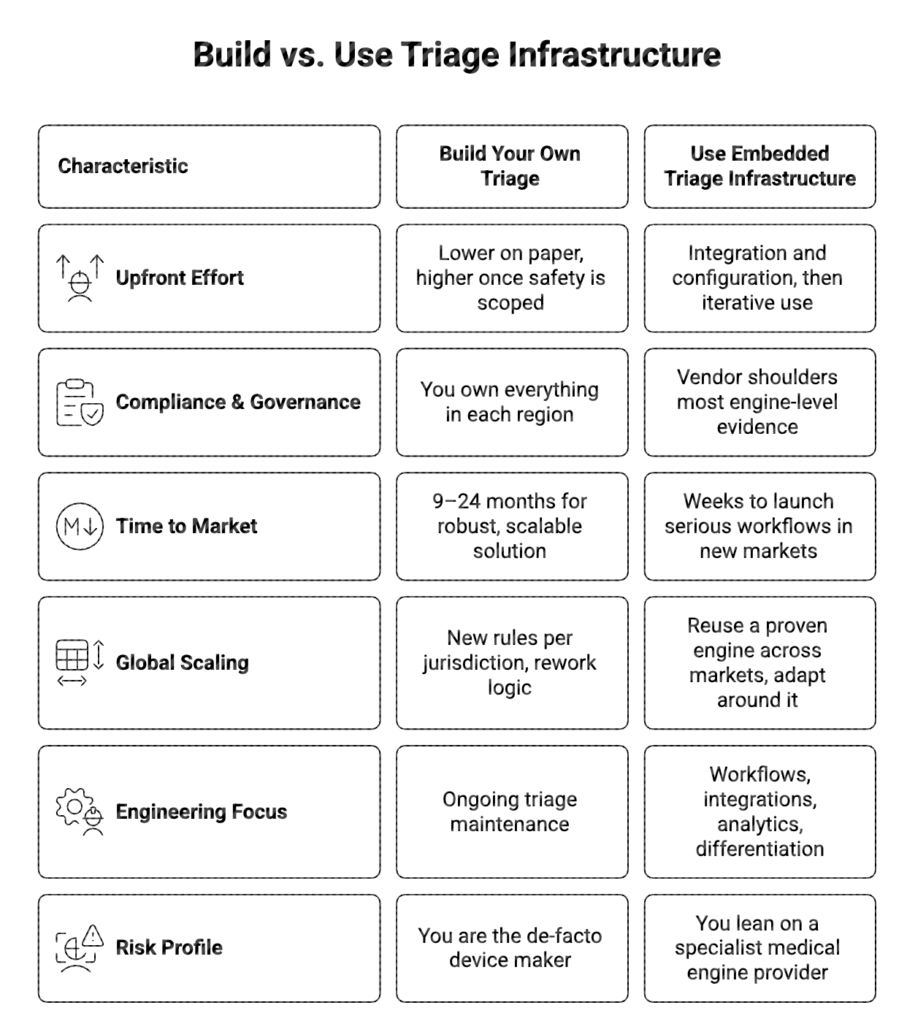
The more countries you target, the more the “build” column grows in cost and uncertainty.
Embedded engines as a global shortcut
A different approach is to treat triage as embedded infrastructure:
- Use a medically supervised, validated engine as the core.
- Integrate it into your product through APIs, iframes, or SDKs.
- Keep your brand, UX, and workflow control.
- Let the engine provider absorb most of the clinical logic and compliance burden.
Done well, this lets you:
- Enter new markets faster because the core triage logic already meets high safety expectations.
- Reuse the same triage primitives while adapting the surrounding workflows and integrations locally.
- Give clinicians and buyers confidence that your triage is built on proven, widely used logic.
You are not giving up control. You are choosing to stand on top of a specialised layer so your team can focus on the parts of the stack that make your product distinct.
How to decide, if you are expanding globally
As a founder, CTO, or product leader looking beyond a single country, ask yourself:
- Does owning triage logic itself materially differentiate your product in the eyes of global buyers?
- Are you prepared to invest in regulatory, clinical, and governance capabilities across multiple jurisdictions?
- Will building triage in house accelerate your international revenue in the next 12–18 months, once you include the compliance and trust work it requires?
If the honest answer to any of these is no, then building triage is not a strategic investment. It is a long‑term tax on your roadmap.
Treat triage as infrastructure.
Let a specialised engine shoulder the burden of safety, validation, and global complexity.
Spend your limited engineering and product energy on the layers where you can truly win: workflow, experience, data, and distribution.
FAQs
1. Why is building a triage engine in house so risky for a global product?
Because the moment your triage influences clinical decisions, it is treated like medical device‑type software in many regions, bringing expectations around safety evidence, governance, and ongoing oversight that grow with every new market.
2. Does this apply even if my product is “just” decision support?
Yes. Clinical decision support tools are increasingly in scope for regulation or at least for stricter internal governance in hospitals and health systems, which means you still face questions on validation, transparency, and risk management.
3. How does using an embedded triage engine help with global expansion?
An embedded engine provides a clinically supervised and validated core that you can reuse across countries, while you adapt workflows, integrations, and UX locally, instead of rebuilding and re‑validating medical logic for each region.
4. Will buying triage mean I lose control of my product?
No. You keep control of your brand, user experience, and workflows, while the engine runs underneath as infrastructure. This lets you focus on differentiation while leveraging a specialised layer for safety‑critical logic.
5. When does it make sense to build triage yourself?
It makes sense only if triage itself is your core product and you are willing to operate as a medical device‑level organisation with the required investment in regulatory, clinical, and governance capabilities across multiple markets.
FAQs
Deploying AI in primary care: Overcoming barriers to AI adoption in general practice
Dr Rony Lindell is Medical Director at Klinik Healthcare Solutions and a practising GP.
The pressures on primary care teams are rising.
The combination of steady growth in patient demand, increased complexity of patient care needs, and limits on the availability of full-time, fully qualified GPs has put efficiency at more of a premium than ever.
Even before the emergence of large language models, artificial intelligence held huge potential for addressing these challenges. AI solutions have a broad range of applications within a typical GP practice, and, in many cases, are already transforming administrative and clinical operations, with benefits felt by clinicians, staff and patients.
For many GPs, however, the understanding of AI’s benefits and potential applications isn’t clear-cut.
As practices struggle with demand on clinical time, factors which serve to slow down the adoption of clinically validated solutions could serve to create additional pressures on clinical and admin teams – leaving them overwhelmed by demand while unable to rely solely on traditional ways-of-working.
AI has the potential to introduce critical efficiencies, save on clinical time, and support clinical decision making – but only if clinicians understand what’s possible, and what’s needed, both from the technical and human sides, to integrate AI into existing workflows and systems.
To achieve this, we need to define what’s possible, where the barriers to adoption lie, and develop the ways-of-working to support effective implementation, as well as the confidence to do so.
What barriers exist to greater adoption of AI in primary care?
The benefits of AI within primary care haven’t gone unnoticed by those in policy and planning roles, for whom new technologies offer the potential to streamline care delivery, transform the management of budgets and allocation of resources, and inform the development of population health management approaches.
Successive documents have highlighted the role of AI in improving patient access to care; NHS England’s Delivery plan for recovering access to primary care, published last year, outlined how AI tools, such as Klinik’s triage and patient flow management tool had been used by York’s Priory Medical Group in order to radically improve access to care.
Despite these examples, barriers to adoption remain. As recently as 2019, a survey of primary care teams found that less than 10% of those surveyed said they were applying AI to reduce or automate administrative tasks.
Resistance to change among primary care teams is holding back adoption
Resistance to change is often cited as one of the key blockers to AI adoption – but the motivations behind it vary, and understanding the varied drivers is critical to improving adoption and delivery enhanced patient outcomes.
AI solutions often fail to support existing workflows, and adaptation is costly.
The introduction of new technologies into clinical practice can be challenging – and while developers should be working closely with clinical and non-clinical representatives of the team to ensure that integration aligns with a practice or Primary Care Networks’ ways of working, adaptation can often be required.
Where teams either struggle to understand the purpose or the benefits of an AI solution, their incentive to adapt may not be great enough to do so. Where adaptation required on the part of the clinician is too significant – often because implementation has been carried out with little regard to existing way of working – clinicians may be resistant.
Integrating AI into existing digital systems may not always be straightforward
The deployment of AI in healthcare typically requires solutions to integrate with existing solutions – either as a standalone solution, typically requiring clinicians to learn and adapt to a new system alongside others, such as their EPR, patient messaging solution, online access platform, or as a backend integration to an existing platform, less visible to the clinician.
In each case, interoperability of systems is needed if the AI is required to pull data to existing systems or to push it to others, such as an EHR. For standalone systems, the workflow issue again adds an additional barrier to adoption, requiring clinicians to add an additional layer to their workflow.
Lack of trust exacerbates these barriers
Finally, a critical factor in the adoption of AI is the extent to which clinicians perceive technologies as reliable; where primary care teams are sceptical about accuracy, or even where they believe tools may not deliver on promises to save time, their willingness to consider adoption may not be sufficient to overcome initial scepticism initial resistance to change.
How to overcome barriers to adoption of AI within primary care
The barriers to adoption of AI within your organisation may include any combination of those outlined above, but typically any plan for implementation requires a similar approach.
Be clear on what it is you are trying to change
The symptoms of patient access challenges take many forms – whether reception staff do not have the capacity to answer an influx of calls at a specific time, or that there aren’t enough appointments to offer one to everyone who needs one, there are few situations where plugging in a new digital solution will solve the problem overnight.
Here, a strategic approach to the adoption of AI is essential to ensure that expectations are managed and that there is a clearly defined purpose for an AI tool. When working with a new practice, we encourage management teams to identify their primary objectives as part of their digital transformation, and work with them to ensure the system enables these.
Help your teams to understand the benefits, and mitigate against potential friction
Whether its your patients or your staff that are resistant to the use of new tools, it’s critical that teams invest resources into bringing people on the journey. Early communication and engagement is critical, to outline what problem is being addressed, how a specific tool may help, and the likely impact – both for the problem, as well as on overall ways-of working.
Implementation should be approached in collaboration with patients and staff, so as to ensure that tools support or enable existing or create new, streamlined ways-of-working, rather than adding additional steps. Training on AI solutions will also help teams to overcome the lack of confidence that often comes from adoption of new solutions – and which may manifest in a resistance to their use.
Involve all staff in the implementation of new technologies – and seek support from digital transformation specialists
Ultimately, the successful adoption of AI in primary care requires an understanding of the key challenges the team is facing, a willingness to test and iterate, and a collaborative approach which involves practice managers, clinical and non-clinical staff, and a supplier that is able to support your practice’s specific needs.
Klinik has supported more than 500 primary care teams to improve access and streamline patient flow management using our AI-assisted triage solution. Our team works closely with practices to help them set clear objectives and develop bespoke clinical pathways, enabled through our online access platform, and guided by specialists in primary care digital transformation.
If you’re interested in exploring how AI could enhance clinical decision-making within your practice, improving access and freeing up capacity within your practice, speak to our team.
Structured, streamlined and collaborative care with a digital front door
As more and more people grow used to the convenience and ease of accessing services online, they’ve come to expect that seeking healthcare should be no different.
In part as a result of the rollout of digital access to primary care through digital tools including the NHS app and practice websites, that expectation is becoming more and more the reality – in London alone, 3 out of 4 people now use digital tools to interact with their GP practice.
For patients this means accessing key features of primary care has become more convenient.
This ease doesn’t just equate to a saving on spent on the phone trying to get an GP appointment, it can change how their enquiry is recorded, triaged, and the relevance of the care they receive.
For this to be the case, the digital front door must be more than just another way to contact your practice – it should support practices to enhance the availability and relevance of care they provide.
When implemented properly, the digital front door becomes a valuable investment for practice teams and primary care networks and can be as beneficial to teams as it is for their patients.
The ‘digital front door’ should be more than just another way of contacting a GP.
For patients, their GP practice is often the first point of contact when they have a concern about their health.
Many continue to see their family doctor as the definitive resource on their health, and their ‘go-to’ healthcare provider in the event they have a problem.
But as demand has risen and staffing patterns continue to change, the expectation that a patient will speak to their GP before anyone else is out of date.
With practices employing many non-GP clinical staff, a GP will not always be the most appropriate clinician to help a patient with their specific problem, nor is it likely they will be the most cost-effective – pharmacists, physiotherapists, nurses, dietitians and others may all be better placed to provide the required care.
In fact, just 44% of appointments offered in primary care last year were with a GP – and a significant number of these could have been avoided, either because no appointment was needed or because a different staff member could have helped instead
More recent developments – such as primary care networks transitioning to the ‘Integrated neighbourhood teams’ model – have seen primary care increasingly serving as a single point of access to a wider range of health and community services – including community mental health and social care.
Triage is an essential feature of online access
However, with increased demand for care and pressure on practice call handling staff to process calls quickly, an initial telephone conversation with reception staff rarely provides enough information on which to make an informed decision of what care will be most appropriate for a patient.
Primary care triage teams often expend considerable resources following up with patients for clarification or may simply book an unnecessary appointment with a GP, taking up precious clinical time and delaying the patient from accessing the most appropriate care.
When implemented effectively, online access doesn’t simply provide a convenient additional channel for patients to access care, it removes the friction for triage teams managing these requests caused by lack of information.
At Klinik, our AI system captures patients’ enquiries through a structured question set, providing teams with differential diagnoses, negative severity symptoms and an urgency assessment. From there, triage teams have a crystal clear picture of the patient’s clinical need and the most appropriate care for that patient.
How to implement a digital front door that enhances access and relieves pressure on your team
Practices have been expected to offer and promote digital access tools to their patients since 2015, and this expectation remains at the heart of the modern general practice model.
Yet many teams have yet to begin using these tools. Other practices we have spoken to have even procured online access tools before opting not to use them, as they failed to solve the problem the practice was seeking to address.
In many cases, they served to increase the complexity of providing access, creating more work and greater confusion for staff, rather than streamlining triage and patient flow management.
When choosing a system for your practice, it’s important to ensure that the system compliments or enhances your pathways, and that it is implemented in a way that reduces, rather than adds to your workload.
Leverage your online access to support better triage decisions
Simply put, your online access solution should enable your triage team to rapidly make a care decision by providing them with the relevant information they require to do so.
Comprehensive patient-history taking for all enquiries enables you to capture all the information a triaging clinician may require, without the need to follow-up with the patient.
For triage teams using Klinik, this information comes accompanied with an initial assessment of need and urgency to support rapid decision-making. The patient’s enquiry, a differential diagnosis, and an assessment of urgency are all displayed to the triaging clinician via the system’s triaging hub, which also enables the case to be directly referred to the relevant team.
By working with practices to implement bespoke care pathways that allow efficient referral to available resources within the practice or PCN, we also ensure that the journey from initial enquiry to the right care is as rapid and accurate as possible.
Capture the same information from phone and from walk-in enquiries for equitable triage
Using online access tools can relieve the pressure on other channels patients use to contact the practice, such as telephone or walk in enquiries. The structured triage processes ensure that care decisions are made based on need, rather than a ‘first-come, first-served approach’.
However, the value your practice derives from using online access as part of triage depends on patients having confidence that their enquiries are treated the same way, regardless of how they choose to contact the practice. For this to be the case, every enquiry must be captured using the Klinik system.
Customers using Klinik for online access and triage also have access to our telephone module, through which call handlers can guide callers through the process of completing the form. Patients who present in-person will be guided through submission by reception staff.
As a result, patients can access care however they choose, but processes ensure all enquiries are treated equitably.
At Klinik we’ve worked with more than 350 UK GP practices and primary care networks to offer enhanced access to primary care for their patients. Through our AI-assisted online triage and patient flow management, we’re helping more patients to access the right care, first time, while saving time and relieving pressures on primary care teams.
Speak to our team to understand how we can support your practice.
How can digital solutions enable truly integrated care
Primary care is in the midst of its most significant period of transformation in decades.
Faced with limited funding and skyrocketing patient demand, the sector has been exploring new opportunities to introduce efficiencies and improve the delivery model for primary care for over a decade.
Charged with delivering more collaborative, integrated healthcare services, primary care networks (PCNs) aim to bring together GP practices with services in the community and secondary care – enhancing collaboration between multidisciplinary teams, and offering patients more straightforward access to a wider range of services.
Many PCNs have sought to become even further integrated into their communities, provide access to healthcare services that meet local needs and improve continuity of care for patients. But PCN managers face a number of barriers on the path to further integration – including difficulties developing new ways of working, gaps in their understanding of demand and capacity, and limited resources to work with.
So how can they overcome these barriers to deliver truly connected care?
Understanding and overcoming key challenges to integration
PCNs still face many obstacles on their road to becoming fully integrated teams: a resistance to change means taking advantage of opportunities to integrate can be slowed, and a lack of digital infrastructure can leave PCN managers essentially working in the dark when it comes to taking decisions needed to improve access and care across the network.
Every practice is covered by a PCN, but the extent of collaborative working varies
SInce 2019, every practice in England sits within a PCN, and 99% of GP practices have signed up to one of these networks.
However, not every PCN has adopted the same degree of integrated working. While many have taken a truly cross-functional approach, a large number of PCNs continue to see only a loose alignment between the practices in the network.
The extent of engagement with other practices, individual procurement decisions, and even variations in the model of triage, may all differ depending on the specific practice. The lethargy of existing workflows and general resistance to adopting new operational methods can often pose significant challenges to change, limiting PCNs’ ability to integrate further.,
Without better information, planning in both the short- and long-term is challenging
The pressures on primary care teams driven by patient demand have continued to rise. The demand for reactive care often presents challenges for primary care teams, many of which aren’t collecting the essential information needed from patients at point of enquiry to appropriately triage their enquiries.
This often means that GPs must deal with a large volume of appointments which may be unnecessary or which could be more cost-effective if handled by a different team member. This presents a significant problem for clinical teams and takes away time that would otherwise be spent on proactive care.
In the long-term, this lack of data creates even larger challenges for PCNs, with staffing decisions often not made on the basis of actual data on demand.
For PCNs, which requires a strategic alignment of objectives and an efficient allocation of resources to cater to the healthcare demands of diverse populations, this lack of information may hinder their ability to do so effectively.
Without effective digital solutions, collaborative working may be limited
A final key obstacle is the lack of alignment around clinical pathways and ways of working between practices within a PCN that may mean opportunities for cross-PCN collaboration are limited – particularly where teams are using different systems or tools for managing patient triage and flow.
Implementing the hub model to integrate primary and community care
For both patients and staff to benefit from the improved access to local care services that PCNs were intended to deliver, it’s essential that services take advantage of opportunities for collaborative working offered by greater integration.
A hub model of triage offers the most straightforward approach to bring together services and streamline patient flow management and collaboration between multidisciplinary teams. Designed to foster integrated primary and community care within PCNs, the hub model centralises triage decisions for patient enquiries across a network, offering clear, consistent care pathways for patients, regardless of at which practice they register their initial enquiry.
Crucially, this model also enables teams to manage follow-up care across the network, and take advantage of all available clinical capacity – including in other practices – to cope with surges in demand.
Digital plays a critical role in enabling effective hub-working for PCNs
In streamlining patient referrals and coordination of care between services, digital tools like Klinik reduces the friction between different providers and ensures rapid collection and sharing of information needed to overcome barriers.
By providing a single digital hub connecting clinicians across a network and which can be accessed by teams regardless of which practice or service they’re based in, Klinik helps PCNs to coordinate patient care and streamline access to a wide range of services across the geographical area.
With AI-assisted patient-history taking providing triage teams with the information needed to make rapid, accurate care decisions, Klinik makes triage and patient flow management more efficient. With all enquiries triaged in a single system, Klinik ensures equitable access to care for patients across the network.
Thanks to the insights contained within the dashboard, PCN managers also have greater oversight of demand and capacity across the network, both at the current time and over a period of months. As a result, they are better able to make decisions on the staffing and resources necessary to ensure patient access within current funding – while also being able to create space for proactive care, too.
The transition toward integrated neighbourhood teams reflects wider pushes toward more sustainable, integrated models of care taking place across healthcare in England.
The hub model of triage is central to enabling true PCN ways of working by helping networks overcome traditional barriers to integration. By embracing these technological innovations, PCNs can enhance service delivery, ensuring patients receive timely, coordinated care.
If you’d like to discuss how Klinik could help your PCN to benefit from a hub-model approach to triage, get in touch with our team to find out more.