In most SaaS categories, building a feature in house is a straightforward trade‑off between time, cost, and flexibility. In healthcare AI, especially triage, the trade‑off adds three extra dimensions:
- Clinical safety and liability
- Regulatory exposure
- Long‑term maintenance and governance
You are not just deciding whether you can build the logic. You are deciding whether you want to live with:
- How that logic behaves in edge cases.
- How clinicians around the world use it under pressure.
- How regulators in different jurisdictions interpret it over time.
This is why many organisations report that the barriers to AI adoption are not purely technical but include regulatory uncertainty and concerns about the maturity and risk of AI tools.
What you are really building when you build triage
You might think you are building a symptom checker. In practice, you are building:
- A clinical decision support system that can fall under medical device rules.
- A global clinical knowledge base that must stay up to date.
- A risk classification engine that handles varied populations and comorbidities.
- A continuous validation pipeline to prove safety in real‑world use.
- A governance and audit function to satisfy hospital, insurer, and regulator questions.
Different regions name the rules differently – for example, FDA guidance for clinical decision support, EU MDR, or national digital health regulations – but the direction of travel is the same: more scrutiny on software that guides clinical decisions. That scrutiny does not disappear just because your team calls it “a feature”.
The global compliance tax nobody scopes
The compliance tax is not a one‑off project. It is an ongoing operating cost that grows with your footprint.
When you build triage in house, you commit to:
- Clinical validation
Showing that your logic behaves safely across age ranges, conditions, and care settings, and updating that evidence as you expand into new markets. - Safety documentation
Producing artefacts that can stand up in front of hospital risk committees, quality teams, and, where applicable, regulators. - Post‑deployment surveillance
Monitoring outcomes, investigating incidents, and demonstrating how you improve the system over time. - Change management
Accepting that every “small tweak” to logic affects a regulated risk surface and may require review, regression testing, and new documentation.
Global expansion multiplies this tax.
What passed a procurement review in one country may raise new questions in another. Two regulators can classify similar software at different risk levels, with different expectations, for the same functionality.
Internal teams consistently underestimate this. Surveys of healthcare organisations highlight regulatory uncertainty, lack of clear governance, and concerns about immature tools as top barriers to AI adoption. Those same issues become your problems the moment you own the triage engine.
Why engineering velocity collapses as you scale
The first version of an internal triage engine usually ships fast:
- Hard‑coded rules.
- Simple branching.
- Manual testing.
Then real requests arrive:
- Cover more age ranges and vulnerable groups.
- Support additional specialties or care settings.
- Adapt flows to fit different provider workflows and cultures.
- Address feedback from clinical champions in each new deployment.
Each change introduces new interactions in your logic and new risk paths to consider. Over time:
- Release cycles slow down because each change requires deeper testing.
- A small group of engineers and clinicians get pulled into constant triage maintenance.
- Roadmaps shift from strategic features to reactive fixes and compliance work.
What started as “two engineers for a quarter” becomes a permanent team whose main job is keeping the triage engine safe, documented, and just good enough to avoid blockers in deals.
The opportunity cost for global health tech teams
The real cost of building triage is not just regulatory work. It is what your team stops doing.
Your competitive edge in global healthcare markets tends to live in:
- How well you integrate into local workflows and systems.
- How you support different care models across countries.
- How you handle multi‑site, multi‑region deployment and analytics.
- How strong your commercial model and distribution are.
Customers rarely choose a platform because its homegrown symptom tree is slightly different. They choose it because:
- It reduces admin and improves capacity.
- It fits how their teams work.
- It meets their risk and compliance expectations without endless negotiation.
Every sprint spent rewriting triage logic for a new country is a sprint not invested in better integrations, better data, or stronger partnerships.
Why triage is infrastructure, not your differentiator
In global healthcare, triage behaves like infrastructure:
- It must be safe.
- It must be consistent.
- It must be predictable and explainable.
That is why more providers and payers expect triage and clinical decision support to meet medical device‑level standards, even where the exact regulatory status varies.
Your defensible IP is far more likely to be:
- The way you orchestrate workflows around triage outputs.
- How you align with each market’s operational reality.
- How you surface insights about demand and capacity to leaders.
- How easy you make it for clinicians to trust and use your product day to day.
Triage itself is a critical building block, but in a global strategy it behaves more like cloud infrastructure or payments than like your core UX.
The real risk when triage goes wrong
When triage fails, the consequences are serious everywhere:
- Patients may be under‑triaged or over‑triaged.
- Clinicians may lose trust in both the tool and your brand.
- Providers may face investigations, and you may be pulled into them.
- Regulators and payers may raise questions that affect future deals.
Studies of AI triage and risk prediction tools in emergency and referral settings highlight the ethical and practical challenges around over‑triage, under‑triage, false positives, and automation bias. These are not abstract issues; they influence how decision makers treat any new AI‑driven triage solution.
Even in jurisdictions where certain decision support software is not tightly regulated, commentary stresses that developers still need robust validation and transparency because oversight frameworks are evolving.s
If you own the triage engine, you own that risk narrative in every market you enter.
Build vs buy: how the comparison changes globally
The naïve calculation:
- Build: engineering cost for a few months.
- Buy: recurring licence plus integration.
The more accurate global calculation:
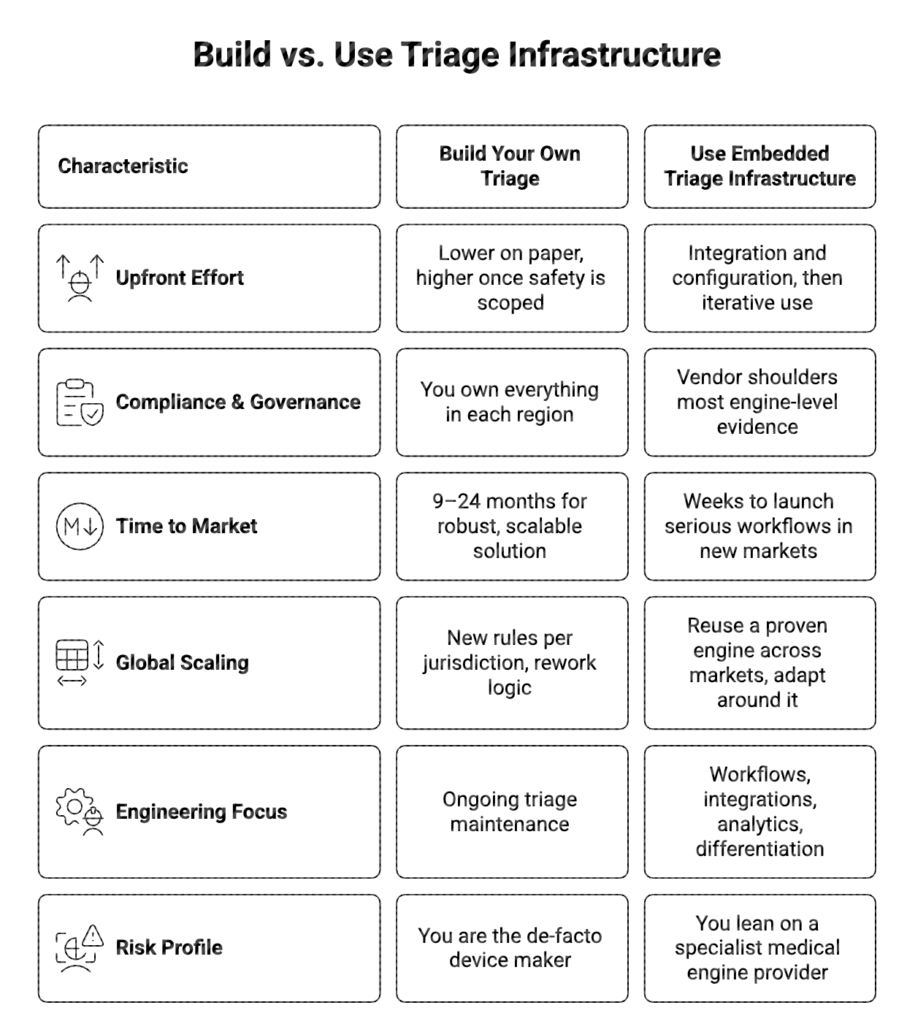
The more countries you target, the more the “build” column grows in cost and uncertainty.
Embedded engines as a global shortcut
A different approach is to treat triage as embedded infrastructure:
- Use a medically supervised, validated engine as the core.
- Integrate it into your product through APIs, iframes, or SDKs.
- Keep your brand, UX, and workflow control.
- Let the engine provider absorb most of the clinical logic and compliance burden.
Done well, this lets you:
- Enter new markets faster because the core triage logic already meets high safety expectations.
- Reuse the same triage primitives while adapting the surrounding workflows and integrations locally.
- Give clinicians and buyers confidence that your triage is built on proven, widely used logic.
You are not giving up control. You are choosing to stand on top of a specialised layer so your team can focus on the parts of the stack that make your product distinct.
How to decide, if you are expanding globally
As a founder, CTO, or product leader looking beyond a single country, ask yourself:
- Does owning triage logic itself materially differentiate your product in the eyes of global buyers?
- Are you prepared to invest in regulatory, clinical, and governance capabilities across multiple jurisdictions?
- Will building triage in house accelerate your international revenue in the next 12–18 months, once you include the compliance and trust work it requires?
If the honest answer to any of these is no, then building triage is not a strategic investment. It is a long‑term tax on your roadmap.
Treat triage as infrastructure.
Let a specialised engine shoulder the burden of safety, validation, and global complexity.
Spend your limited engineering and product energy on the layers where you can truly win: workflow, experience, data, and distribution.
FAQs
1. Why is building a triage engine in house so risky for a global product?
Because the moment your triage influences clinical decisions, it is treated like medical device‑type software in many regions, bringing expectations around safety evidence, governance, and ongoing oversight that grow with every new market.
2. Does this apply even if my product is “just” decision support?
Yes. Clinical decision support tools are increasingly in scope for regulation or at least for stricter internal governance in hospitals and health systems, which means you still face questions on validation, transparency, and risk management.
3. How does using an embedded triage engine help with global expansion?
An embedded engine provides a clinically supervised and validated core that you can reuse across countries, while you adapt workflows, integrations, and UX locally, instead of rebuilding and re‑validating medical logic for each region.
4. Will buying triage mean I lose control of my product?
No. You keep control of your brand, user experience, and workflows, while the engine runs underneath as infrastructure. This lets you focus on differentiation while leveraging a specialised layer for safety‑critical logic.
5. When does it make sense to build triage yourself?
It makes sense only if triage itself is your core product and you are willing to operate as a medical device‑level organisation with the required investment in regulatory, clinical, and governance capabilities across multiple markets.


